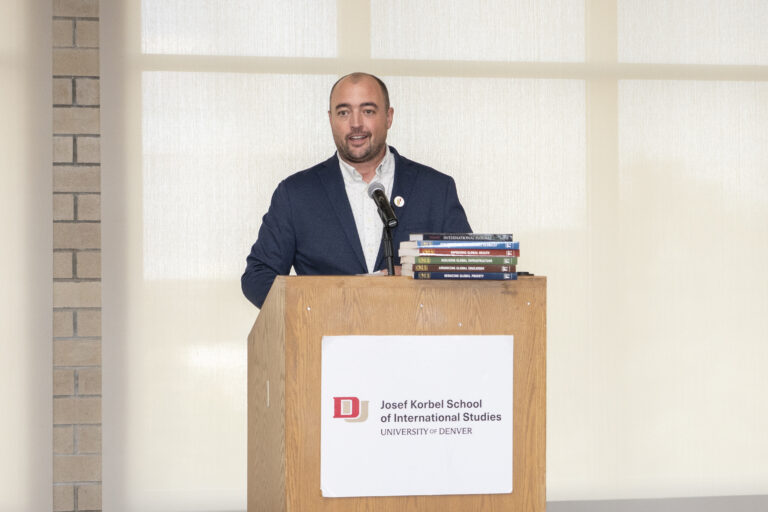
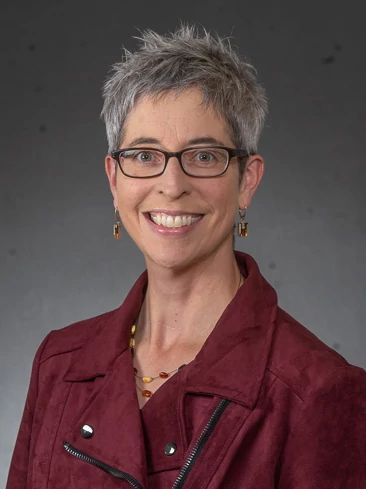
DENVER — As a psychology professor and associate vice provost of public good strategy and research at the University of Denver, Anne DePrince, Ph.D., has focused her career on studying the devastating effects of intimate partner violence, known as IPV..
“My research is broadly on intimate violence and its consequences, and in particular, my team looks at multidisciplinary responses to intimate partner violence,” DePrince said. “What I mean by intimate violence … it can take many forms that could be something like sexual assault or intimate partner abuse, maltreatment of older adults or children, and we know that much intimate violence disproportionately affects girls and women, so our work has has done a lot to look specifically at violence against women.”
A clinical psychologist by training, DePrince and her colleagues have studied the links between IPV and depression and post-traumatic stress disorder, as well as impacts on education and the ability to work.
“A lot of our work has been in partnership with community- or system-based agencies,” DePrince said. “For instance, I’ve worked a lot with the Denver District Attorney’s office and the police department to try to bring research to bear on pressing questions they have about how communities should be responding to intimate violence, and what could we be doing to better collaborate and coordinate responses to meet the many needs that survivors can have an aftermath of violence.”
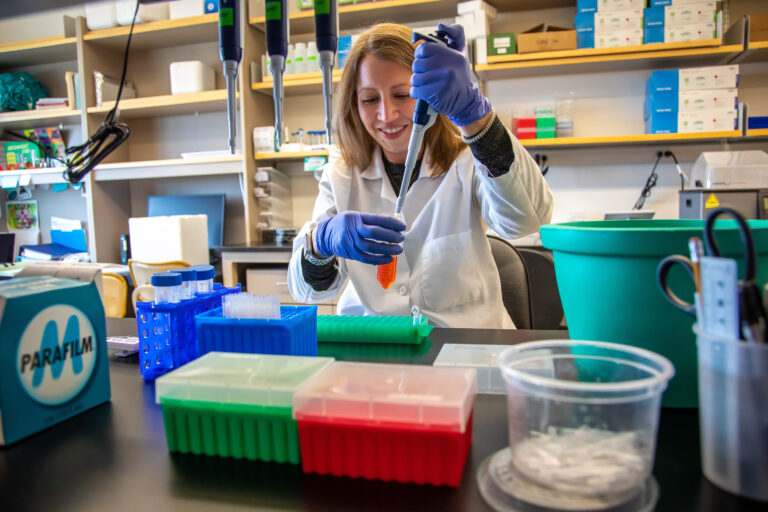
In recent research, DePrince has teamed with an ideal collaborator in Eileen Wang, M.D.,, an allergist and immunologist with National Jewish Health in Denver who is also on the faculty of the University of Colorado School of Medicine in Aurora.
Wang worked with victims of IPV before embarking on her career in medicine. She joined National Jewish in 2014 and has worked on a number of research initiatives involving medical outcomes associated with IPV, including a 2021 study that found that victims of IPV typically had worse asthma outcomes.
That raised questions that led to a study they co-authored with several others, “Uncontrolled Asthma, Intimate Partner Violence, and Inflammatory Pathways: Surprising Insights From Cytokine Profiles,” published by Allergy journal in July 2025. The study was in part funded in part by the University of Denver/National Jewish Health Seed Money Collaborative Research Award, which awarded the project a microgrant in 2021. The study gauged the presence of cytokines and other biomarkers of inflammation in patients with uncontrolled asthma. Nearly half of the patients had experienced IPV at some point.
The results were a bit of a surprise to both Wang and DePrince. “The long and the short of that paper is that people who indicated they’d been victimized by an intimate partner were showing a really different inflammation pattern than you’d expect, relative to people in this sample who hadn’t been victimized by an intimate partner,” DePrince said. “Where there is usually a lot of inflammation linked with asthma, this group was showing, by comparison, really low inflammation, so it raises some interesting questions.”
“We were rather shocked to have these findings,” Wang said. “When we initially presented this, this was not what our hypothesis was at all.”
DePrince hypothesized that the results were tied to dysregulation stemming from IPV. “One of the things that we see is that trauma often goes with dysregulation, and sometimes it’s hard to predict which direction that dysregulation will be in,” she said. “There’s been research from others across the country and also colleagues here at DU showing that part of our stress response system in response to trauma can end up over- or underactivated, so you could have this dysregulation in either direction.
“So while the finding was surprising, in thinking about it afterwards, I think Eileen and I are very curious: Is it? Is it the case that this is part of that larger pattern we’ve seen that trauma leads to dysregulation, sometimes in unexpected directions?”
Outside of asthma research, studies on IPV and inflammation have shown “inflammatory pathways that look normal at baseline, but when they get a trigger, they react abnormally,” Wang said. “We need to dig into it, because it has direct implications for all the expensive treatments we do for asthma and all the progress and movement we’ve had with our aim towards these inflammatory pathways.”
Echoed DePrince: “For us, this study suggests there’s a lot more questions to ask about timing of intimate partner abuse, severity, frequency, things that we know from other research can make a difference for health outcomes.”
“A lot of the medications designed to control asthma are designed based on the biology of inflammation,” she added. The new study’s results “suggest, if there’s a different disease course for patients who have a history of intimate partner abuse, that those go-to medications designed to address inflammation may not be the right tool, and that might be part of the reason that you see more uncontrolled asthma among people with a history of intimate partner abuse.”
To that end, Wang and DePrince are involved in ongoing research investigating IPV’s effects on additional inflammatory pathways and neuropeptides. The latter research is complete, but needs further analysis before publication, Wang said, noting, “We’re seeing some patterns, mostly with one neuropeptide.”
“This is not an uncommon phenomenon,” Wang said, adding that 40% to 50% of National Jewish’s patients report experiencing IPV. “We absolutely need to do better for them. We need to figure out what is going on and what could actually work for them.”
“We have established bad outcomes and now this interesting inflammatory profile,” she added. “Now we need to fill in the middle: How does that happen? And where is the target for treatment?”